Patient preparation, safety
and hazards in imaging
infants and children
Jacqueline M Pennock
Chapter Contents
- Introduction
- Imaging team
- Assessment of patients for imaging
- Organizing the day
- Preparation of the MR unit and scanning room
- Clinical safety in the MR unit
- Physiological monitoring devices
- Prior to sedation
- Sedation
- Transfer to the MR unit
- Monitoring
- Immobilization
- During the scan
- Recovery from sedation
- Technical considerations
- Summary
- Acknowledgments
- References
Introduction
‘The two greatest obstacles we face in imaging infants and children are the proper preparation of the subject and the selection of the right combination of imaging parameters to achieve the desired result’3.
Magnetic resonance (MR) systems are designed to accommodate the adult population; however, with a little effort and careful planning they can be successfully used to scan infants and children. This chapter offers advice about patient preparation and imaging protocols for those faced with the prospect of scanning infants up to 2 years of age in scanners used mainly for adults.
Examples of the documentation we use for each pediatric examination are included as a guide for the reader with only occasional access to a scanner. We find this information extremely useful for follow-up studies, quality assurance in our sedation program, and dealing with potential medico-legal problems.
< prev | top | contents | next >
Imaging team

Fig. 1.1 ‘the Duchess was sitting on a three-legged stool in the middle, nursing a baby; the cook was leaning over the fire, stirring a large cauldron which seemed to be full of soup’. Care and understanding are required for preparing an anxious mother and child for imaging.
Examining a sick infant is a team effort and involves close co-operation between clinical and imaging staff as well as the mother and infant. A highly motivated and unified clinical team helps make a potentially distressing event easier for the mother and child (Fig. 1.1). Our current core team consists of two pediatricians, a radiologist, pediatric nursing staff in the children’s out-patients and a radiographer with training in pediatric imaging.
Our team members are involved in all aspects of patient care including setting up new imaging protocols and reporting images.
< prev | top | contents | next >
Assessment of patients for imaging
Before an MR appointment is made the infant is seen by a pediatrician who takes a medical history including details of previous operations and possible implants. If, for example, a ventriculo-peritoneal shunt or a patent ductus arteriosus clip is present then its magnetic compatibility is checked before an appointment is given. The book by Shellock and Kanal lists many items, which have been tested for attraction/ deflection forces during exposure to static magnetic fields. These authors are also accessible through the world wide web and provide a quick reply to questions and problems concerned with safety14.
At this initial assessment the pediatrician explains the MR procedure, the sedation protocol and gives instructions on feeding and or fasting before the scan. We recommend that the infant has no food for 4h and no drink for 2h before sedation. The parents are asked to prevent their infant from falling asleep for at least 2h before the scan. If possible we schedule appointments to coincide with the natural sleeping pattern of the infant.
< prev | top | contents | next >
Organizing the day

Fig. 1.2 ‘the Rabbit actually took a watch out of its waistcoat-pocket, and looked at it and then hurried on’.
It is not possible or desirable to rush mothers and babies through a scanning day.
Scheduling naturally sleeping and sedated infants can be difficult and requires a degree of flexibility. It is much easier to have exclusively pediatric scanning sessions. Studying babies even when sedated takes more time than adults and they cannot be rushed (Fig. 1.2).
Patients coming from home are given appointment times and admitted to a children’s day care ward whereas in-patients are booked at times convenient to the ward.
We offer the parents the opportunity to be with their child throughout the preparation for the scan and encourage them to accompany the baby to the imaging unit so that they can see their child is asleep and comfortable in the scanner. They can stay beside their infant in the scanner if they wish; however, they are often happy to have some time to themselves while we look after their child. Parents going into the scanner room need to be carefully metal checked.
< prev | top | contents | next >
Preparation of the MR unit and scanning room

Fig. 1.3 ‘The rabbit started violently, dropped the white kid gloves and the fan and skurried away into the darkness as hard as he could go’. At first sight an MR scanner can be a frightening piece of machinery.
Although the sleeping child is unaffected by the sight of an MR scanner, for a new and anxious parent it can be a distressing experience (Fig. 1.3). We attempt to make the scanning room a less intimidating place before a pediatric session by changing the standard hospital linen to brightly colored baby blankets, with flannelette sheets and duvets for cosiness and warmth. We have our own washing machine in the unit so the bedding is washed on site and does not disappear into the depths of the hospital laundry. Removable plastic nursery rhyme characters can be placed around the magnet for the baby scanning day. A comfortable plastic chair placed next to the magnet is useful for parents to nurse the baby to sleep before the scan.
We put some toys and books in the waiting room for brothers and sisters to play with while their sibling is being examined. We also have coffee and tea facilities available in the waiting room. These details are designed to provide a relaxed environment for parents and their infants.
< prev | top | contents | next >
Clinical safety in the MR unit
To manage any emergencies arising from scanning sick and sedated infants adequate resuscitation equipment must be available in the MR unit and all the members of the imaging team must be trained in its use.
The minimal requirements for resuscitation are a positive-pressure oxygen delivery system with the appropriate flow meters, wall suction with an assortment of catheters suitable for small children, and physiological monitoring. Back-up portable oxygen cylinders and suction boxes should be available outside the scanning unit. An emergency resuscitation box containing ‘in date’ drugs and appropriately sized and magnetically safe laryngoscopes, oral airways and positive pressure bags should be in the scanning room or close at hand1.
< prev | top | contents | next >
Physiological monitoring devices
These may be either situated in the scanning room or outside in the control room. Monitors in the scanning room may need to be shielded to prevent radiofrequency (RF) interference. If free standing, they should be attached to the wall with a plastic chain, well behind the 5-Gauss line.
Although our equipment is checked for safety on a regular basis we take the extra precaution of checking that all the equipment used for scanning babies is in the unit and working before we start each day’s scanning (Table 1.1).
< prev | top | contents | next >
Prior to sedation
SAFETY IN THE PRESENCE OF A MAGNETIC FIELD

Fig. 1.4 ‘At this the whole pack rose up into the air and came flying down upon her; she gave a little scream, half of fright and half of anger and tried to beat them off…’. The missile effect on pocket contents and other ferromagnetic materials in the presence of a magnetic field is both dangerous and terrifying and can be fatal.
It is essential that all patients and accompanying persons are thoroughly screened before entering the magnetic field. Various types of screening are necessary and we use a series of metal check forms for visitors and different types of patients. A well-taken clinical history should reveal any metal or electronically activated implants in the child. However, before any sedation is given, a formal metal check form for the baby (Table 1.2) should be completed by an informed and MR-aware member of staff.
At the same time earrings and hair ornaments as well as clothes with metal buttons and religious artifacts should be removed. Baby-grows and clothes with metal poppers are not suitable attire for an MR scan. A hospital flannelette nightie with tie or velcro fastenings is ideal, leaving the feet free for attaching pulse oximeter probes and the chest accessible for ECG leads.
It is also essential that the person accompanying the baby throughout the procedure completes and signs a metal check form (Table 1.3). In our unit all new members of staff complete and sign a screening form as part of their clinical induction for relevant medical history on arrival in the unit. Staff who visit the unit only on pediatric days may need to be under constant vigil and are always reminded to empty their pockets and remove watches before they enter the scanner room (Fig. 1.4).
CLINICAL CARE
On the day of the MR appointment the mother and child are seen in the day care ward by the pediatrician and the pediatric nurse. The infant is weighed and his or her body temperature, pulse rate and respiratory rate are recorded by the pediatric nurse on the drug chart (Table 1.4). The pediatrician performs a physical examination on the child and checks for signs of upper respiratory tract infection or any other current illness which may preclude sedation.
The infant’s normal sleep pattern and general levels of activity are also noted and any sleep-related problem such as snoring, stridor or apnea is documented (Table 1.5). Supplemental oxygen may be needed when the child is sedated if there is a history of chronic lung disease, prematurity or snoring.
< prev | top | contents | next >
Sedation

Fig. 1.5 ‘so Alice ventured to taste it, and finding it very nice she soon finished it off’. However chloral hydrate does not taste very nice.
Chloral hydrate is the most popular and frequently used sedative in radiology today8. It is readily available, easily administered and has a relatively wide margin of safety4, 8. We have scanned over 1000 infants whose problems cover all five physical status categories of the American Academy of Pediatrics1 with chloral hydrate
2, 8.
Occasionally, children over 1 year of age become hyperactive with oral chloral hydrate and if this happens we use nasal midazolam 0.2–0.5mg/kg
9,
11,
12
or pethidine compound 0.06ml/kg intramuscularly and oral trimeprazine (alimemazine) (Vallergan) 4mg/kg. Other drugs have been used with or without chloral but whatever the decision, it is recommended that each unit sets up its own formulary and keeps the number of drugs used to a minimum3.
Oral chloral hydrate is best given on an empty stomach as it is rapidly absorbed and most children are asleep within 15–30min of administration. We recommend that chloral is given slowly from a syringe into the side of the mouth with the infant semi-upright in the mother’s arms. However, it tastes awful and some infants will spit it out. With patience and care it is usually possible to ensure that most of the dose is swallowed (Fig. 1.5).
Infants with muscle disorders or generalized hypotonia are given a smaller dose of sedation, calculated on an individual basis.
We have found vomiting to be a problem only in the period immediately after the administration of the chloral, and not when the child is asleep if the infant has been properly prepared.
Chloral hydrate suppositories are useful for the child who is upset by the oral preparation. However, rectal applications may cause a bowel movement and then additional drugs may be required.
The doses and preparations we have found to be most successful are given in Table 1.6.
Infants less than 6 weeks of age are scanned whenever possible during natural sleep after a feed. If, however, these young babies do not sleep then a smaller dose of either oral or rectal chloral hydrate can be given (Table 1.6).
The dose and route of sedation are determined by the pediatrician (Table 1.4). The sedation should only be given when the radiographer performing the imaging has confirmed that the scanner is free and working, and that he or she is ready to scan the infant.
< prev | top | contents | next >
Transfer to the MR unit
When the sedation has been given and the infant is settled we attach a pulse oximeter probe and put the baby into a small baby cot with wheels. The mother and the baby are then taken to a quiet area in the MR unit until the baby falls asleep.
Immediately before entering the scanning room we do a final metal check and ask the accompanying person to empty their pockets and remove watches, etc. It is also worthwhile checking the baby again before putting him or her into the scanner as religious artifacts may have been put back on the baby or hidden in their clothes.
< prev | top | contents | next >
Monitoring
Monitoring of sedated and naturally sleeping infants during an MR scan is mandatory. MR-compatible monitoring systems are available for this purpose and can be purchased separately or directly from the MR manufacturer. The monitoring equipment accessories should be of the correct size for the infant and approved and tested by the MR manufacturer.
We use both pulse oximetry and ECG. ECG electrodes should be carefully placed on the chest and have no contact with each other. The ECG leads should be plaited and pass along the long axis of the body and out of the coil and have as little contact with the skin as possible.
The pulse oximeter should be attached to the infant’s foot so that the probe and lead are outside the receive coil. Coiled monitoring wires may cause skin burns in rapidly changing magnetic fields10.
< prev | top | contents | next >
Immobilization
Fig. 1.6 ‘and put her hands over her ears, vainly trying to shut out the dreadful uproar’. Gradient noise can disturb a sleeping infant.
Sedation alone may not keep an infant still enough to obtain diagnostic images. Swaddling further reduces body movement and helps to keep the infant warm. We routinely scan babies on their side, this position reduces the artifact from breathing and snoring and also prevents inhalation of secretions. If, however, the baby objects then it is better to let them settle into their preferred position and accept that getting the images straight can be achieved with the pilot scans.
We cover a vacuum-pack bag (Vac-fix)15 containing tiny polystyrene granules with a muslin baby nappy and curl the bag around the baby’s head. When the air is evacuated from the bag the head is cradled in a firm but gentle mold. This device also protects the ears from the noise of the gradients (Fig. 1.6) and heat loss through the scalp is minimized. In very small babies it may be necessary to provide extra warmth and well-insulated gel or wheat-filled heated bags are suitable for this purpose.
Before the baby is slid into the scanner the monitoring is checked. Infants who snore or suffer from broncho-pulmonary dysplasia or have pronounced hypotonia may require oxygen to maintain their saturation levels. In these cases we attach a small ventilation mask to the oxygen supply and place the mask close to the infant’s face before sliding them into the magnet and the oxygen flow can then be adjusted without bringing the baby in and out of the magnet.
< prev | top | contents | next >
During the scan
Oxygen saturation and heart rate are recorded at 5-min intervals throughout the scan by the pediatrician (Table 1.7). He or she knows the clinical state of each infant and is responsible for the procedures of evacuation, resuscitation and the management of any reaction to the sedative and/or contrast agents.
Although each member of the group has his or her own skill we have an agreed protocol for the responsibilities of all team members to cover emergencies including a quench of the magnet. An example of the protocol we use in the event of a respiratory or cardiac arrest is given in Table 1.8.
Any unexpected event, although extremely rare, should be well documented and a careful explanation given to the parents. Precautions need to be taken so that infants over 6 months of age do not wake up and come out of the bore of the scanner and fall off the scanner table on to the floor.
< prev | top | contents | next >
Recovery from sedation
Most sedated infants will waken up naturally as they are brought out of the magnet; however, if this is not the case the baby should either stay in the MR unit or return to the ward with supervised monitoring continued until he or she is rousable.
The recommended discharge criteria after sedation are that the child must return to the baseline established prior to receiving sedation and this will depend on the developmental level of the child1.
Discharge can be considered safe if the baby is rousable and orientated with stable vital signs and able to take a drink.
We give the parents written instructions about care of their child after the examination with information on the sedation, other relevant details and a telephone number in case of an emergency (Table 1.9).
< prev | top | contents | next >
Technical considerations
COILS

Fig. 1.7 ‘the last time she saw them, they were trying to put the Dormouse into the teapot’. Always use the smallest coil for the part being examined.
The signal to noise ratio on an MR image is greatly improved by using the smallest coil (‘closest fit’) for the part being examined (Fig. 1.7). Preterm and term neonates can be imaged in the adult knee coil (typical internal diameter 19cm).
If small children are expected to become a significant proportion of your work load then purchasing a head coil with an internal diameter of 24cm is recommended for infants aged from 2 months to 2 years of age. We have found our home-made split coil made from clear perspex excellent for this age group (Fig. 1.8). The improvement in the signal to noise ratio, the shorter scanning times and ease of positioning the infant within this coil makes it an excellent investment.
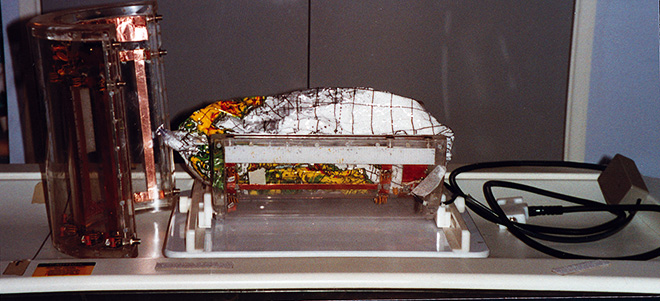
Fig. 1.8 The ‘in house’ transparent split coil with an internal diameter of 24cm. Inside the coil is an inflatable plastic globe filled with small polystyrene balls which is our home-made fixation device.
SEQUENCE CHOICE AND IMAGING PROTOCOLS
It is not possible to rush infants through an MR examination and there is always the risk that the baby will waken at any time. Before the infant is put into the scanner we make sure we have the relevant clinical information, and if possible a provisional diagnosis so that the appropriate sequences can be entered onto the computer prior to the examination.
At birth the water content of the infant’s brain is 92–95% and during the first 2 years of life falls to the proportions of the adult brain, that is 80–85%7. This is associated with a markedly increased T1 and T2 and the standard sequences for the adult brain are not appropriate for imaging infants. It is important to adjust the available adult sequences to accommodate the changes in T1 and T2 as physiological myelination and growth take place. A list of sequence parameters for imaging the central nervous system in infants up to the age of 2 years is given in Table 1.10 for systems operating at 1.0 Tesla.
The brain changes rapidly from birth to 2 years of age16,17 and being aware of these changes and their appearance on your own machine will help in the differentiation between normal development and the presence of pathology. Compiling a file of ‘normal’ images throughout the brain with a variety of sequences at different ages is a useful and informative exercise.
IMAGING PROTOCOLS
In preterm and term infants we start all examinations with a short TR, short TE spin echo sequence in the transverse plane. It takes less than 5min and provides information on ventricular size and shape, brain swelling, hemorrhage and cystic change.
The second sequence is usually a long TR, long TE spin echo or a fast spin echo in the same plane and with the same slice thickness and field of view. These two sequences may give enough information for a diagnosis. If the baby remains asleep we obtain other useful sequences. An example of the parameters of conventional sequences is given in Table 1.11.
OTHER SEQUENCES IN SPECIFIC CONDITIONS
The image contrast in diffusion-weighted sequences depends on the molecular motion of water. These sequences show regions of focal infarction and diffuse anoxic–ischemic brain injury during the early phase which are not obvious on T1 and T2 weighted spin echo or inversion recovery images6.
If a new-born infant has a history of suspected infarction or hypoxic–ischemic encephalopathy and is being scanned within 48h of the event we follow the short TR TE spin echo sequence with diffusion-weighted sequences.
Angiographic sequences are not so useful in the new-born infant as cerebral blood flow is slow and the blood vessels are small. However, they may be very useful in the older infant for defining the blood flow.
The FLAIR (fluid attenuated inversion recovery) sequence is particularly sensitive for the detection of subdural hematomas in the new born13. In the older infant this sequence provides excellent information on regions of gliosis and pathology at the CSF interface18.
SPECIAL CONSIDERATIONS
Sick ventilated infants can be imaged safely in a distant MR unit provided the same level of care is available as that in the neonatal intensive care unit. Extra preparation and safety precautions are necessary including a specific metal check form (Table 1.12). Monitoring of body temperature may be required and this is not a problem as long as the temperature probe has been tested for use in a magnetic field. Arterial and venous lines need to be lengthened so that pumps and monitoring devices can be parked safely behind the 5-Gauss line. Ventilator tubing and oxygen lines should be prepared and in situ before the baby arrives in the unit.
In our hospital the baby is brought from the intensive care unit in a standard Vickers transport incubator. The incubator is parked and locked in a corner of the room well beyond the 5-Gauss line and attached to the wall by a plastic chain. The infant is ventilated from the Vicker neovent unit via long extension tubes from the incubator to the baby. Appropriate adjustment of the inspiratory and expiratory pressure is required to take account of the large dead space. Alternatively infants can be imaged using an MR-compatible ventilator (Siemens).
CONTRAST AGENTS
The use of gadolinium-based contrast agents may be indicated in defined clinical conditions in infants, for example in infections and suspected tumors.
If there is a possibility that a contrast agent will be required then an intravenous line should be inserted prior to sedation and after the application of a topical anesthetic cream such as EMLA.
< prev | top | contents | next >
Table 1.1 List of equipment to be checked at the beginning of each pediatric session
| Check that | Checked |
|---|---|
| Piped medical gases have appropriately sized flow meters attached | |
| Extra portable gas cylinders are close by and full | |
| Portable suction is available, working and catheters are available | |
| The insulation on the transmit and receive coils is not damaged | |
| All monitoring equipment is working and sufficient probes and leads available | |
| The insulation on ECG and pulse oximetry leads is not broken | |
| Contents of pediatric resuscitation box are there | |
| Drugs are not out of date | |
| Scanner working | |
| Other...... |
< prev | top | contents | next >
Table 1.2 Final metal safety check for imaging infants (use in combination with Table 1.12 if relevant). Some categories from Shellock and Kanal14.
| Name: | Date: | ||
|---|---|---|---|
| Categories | Yes | No | |
| Cardiac pacemaker – any type | |||
| Heart surgery (e.g. patent ductus) or other | |||
| Ventriculo-peritoneal shunt | |||
| Other surgery | |||
| Any type of surgical clip or staples | |||
| Aneurysm clip | |||
| Any type of biostimulator or neurostimulator pump | |||
| Any type of internal electrode including pacing wires, cochlear implant, other | |||
| Swan–Ganz catheter | |||
| Any type of electronic, mechanical or magnetic implant | |||
| Hearing aid or any type of ear implant | |||
| Any type of foreign body, shrapnel or bullet | |||
| Implanted drug infusion device | |||
| Orbital/eye prosthesis | |||
| Any type of implant held in place by a magnet | |||
| Artificial limb or joint | |||
| Any implanted orthopedic item | |||
| Allergies | |||
| Remove earrings and all jewelry | |||
| Remove ornaments | |||
| Change into hospital gown | |||
|
If the answer to any of the above questions is ‘YES’ please give details. Please note: that a device not known to be safe must be assumed to be unsafe. In the cases operated by microprocessors (e.g. implantable pumps) device malfunction caused by field effects on the circuitry must be considered. Other devices such as ventricular shunts, orthodontic braces may be safe, but may degrade image quality significantly. | |
| Name: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . | Date: . . . . . . . . . . . . . . . . . . . . . . . . |
| Signed:. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . | (Parent or guardian) |
| . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . MR personnel | |
< prev | top | contents | next >
Table 1.3 Imaging safety check list for parent/guardian/accompanying person. Some categories from Shellock and Kanal14. This form is offered as a guideline and can be changed to meet individual requirements.
| Name: | Date: | ||
|---|---|---|---|
| Categories | Yes | No | |
| Cardiac pacemaker any type | |||
| Aneurysm clip | |||
| Any type of biostimulator or neurostimulator pump | |||
| Any type of internal electrode including pacing wires, cochlear implant, other | |||
| Implanted insulin pump | |||
| Any type of electronic, mechanical or magnetic implant | |||
| Hearing aid | |||
| Implanted drug infusion device | |||
| Any type of foreign body, shrapnel or bullet | |||
| Any type of ear implant | |||
| Artificial eye | |||
| Occupation as a metal worker, grinder, welder | |||
| Any type of implant held in place by a magnet | |||
| Vascular access port | |||
| Intraventricular shunt | |||
| Artificial limb or joint | |||
| Any implanted orthopedic item | |||
| Pregnancy | |||
| Before entering the scanning room | |||
| please remove your watch | |||
| please take out metal hair ornaments | |||
| please empty your pockets (some coins are ferromagnetic) | |||
|
If the answer to any of the above questions is ‘YES’ please give details. Please note: that a device not known to be safe must be assumed to be unsafe. In the cases operated by microprocessors (e.g. implantable pumps) device malfunction caused by field effects on the circuitry must be considered. Other devices such as ventricular shunts, orthodontic braces may be safe, but may degrade image quality significantly. | |
| Name: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . | Date: . . . . . . . . . . . . . . . . . . . . . . . . |
| Signed:. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . | (Parent or guardian) |
| . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . MR personnel | |
< prev | top | contents | next >
Table 1.4 Drug chart and vital signs before MR procedure
| Name: | Date: |
| Vital signs |
| Temperature | Respiratory rate | Pulse rate | Body weight |
| Drug prescribed | Dose/kg | Actual dose | Route oral/rectal |
| Time of administration: |
| Problems with administration: |
| None | Coughing | Vomiting | Bowel movement | Other |
| Pediatrician/nurse: | Date: |
< prev | top | contents | next >
Table 1.5 Pediatric record form for magnetic resonance studies
| Name Date of birth Consultant |
Examination date Time |
||
| Part to be examined | |||
| Reason for MR study | |||
| Is contrast required yes/no | EMLA applied or iv in situ | ||
| Previous MR studies yes/no | When | ||
|
Relevant past medical history Problems yes/no Details |
Previous operations yes/no Implants yes/no Details Checked for magnetic compatibility yes/no |
||
|
Previous sedation yes/no Problems yes/no Details |
|||
| On-going problems | |||
| Oxygen requirement | Feeding/swallowing difficulties | Snoring | Other |
| Present condition enter times below please | |||
| Last food | Last drink | Last sleep | Last bowel movement |
| Signs of respiratory tract infection yes/no | Other illness yes/no | ||
| Current medication | |||
| Metal check internal yes/no | Metal check external yes/no (hair, ears, jewelry, clothes changed) | ||
| Intravenous lines long enough yes/no | |||
| Magnet safe yes/no | |||
| Signed | |||
< prev | top | contents | next >
Table 1.6 Age-related doses for oral chloral hydrate
| Age | Dose |
| Up to 6 weeks post term | nil or |
| (46 weeks PMA) | chloral hydrate 30–50mg/kg |
| 47 weeks PMA – 6 months | chloral hydrate 50–80mg/kg |
| 7 months – 2 years | chloral hydrate 80–100mg/kg (maximum dose 2g) |
| PMA, postmenstrual age | |
| Readily available preparations of chloral hydrate: | |
| Oral | 200mg/5ml flavored with blackcurrant |
| Suppositories | 12.5, 25 and 50mg available on most neonatal units |
< prev | top | contents | next >
Table 1.7 Oxygen saturation measurements during MR imaging
| Name: | Date of birth: | Date: |
| Start time | |
| Baseline O2 saturation | |
| Baseline pulse rate |
| Time from start of scan | O2 saturation | Pulse rate | Time from start of scan | O2 saturation | Pulse rate |
| 5 | 35 | ||||
| 10 | 40 | ||||
| 15 | 45 | ||||
| 20 | 50 | ||||
| 25 | 55 | ||||
| 30 | 60 |
| Monitoring normal/abnormal (specify) | Oxygen required yes/no |
| Amount |
| Contrast given | type | dose | ||
| Adverse reaction | ||||
| Time of wakening: | Normal O2 saturation in air | Drinking yes/no | ||
| Injection site checked yes/no | Sent to ward/home | |||
| Discharge letter given to parents | yes/no | |||
| Signed by pediatrician: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . |
| Time: . . . . . . . . . . . . . . . . . . . . . |
< prev | top | contents | next >
Table 1.8 Protocol for evacuation of MR scanner
In the event of a respiratory or cardiac arrest:
- Remove the infant from the magnet and the MR room
- Assigned person closes door to MR room (to prevent access by unauthorized personnel (such as cardiac arrest team)
- Place on a stretcher outside the MR room
- Assigned person puts out cardiac arrest call
- Pediatrician starts cardio-pulmonary resuscitation
- Assigned person attaches mobile pulse oximeter
- Assigned person makes ready suction with correct-sized catheter, drugs, oxygen with mask and ambu bag, intubation equipment, intravenous access equipment, etc.
In our hospital the assigned person is the radiographer.
A written report of any incident must be produced. Careful explanation to the parents is also required.
< prev | top | contents | next >
Table 1.9 Patient information sheet
Hospital address and name of department
Telephone numbers
Dear parents/carers
Your infant has been sedated today with a drug called . . . . . . . . . . . . . . . .
He/she also had an injection of a contrast agent to enhance the images.
There were/were not any problems.
Your child may remain sleepy for up to 8h but you should be able to waken
her/him easily and he/she may be irritable for up to 24h after this sedation.
Eating and drinking instructions: we suggest that you feed your baby with juice, formula or breast milk. If there is no signs of vomiting then continue with your usual routine.
If you are anxious about any aspects of the baby’s activity please do not hesitate to ring the hospital at the above telephone number.
The results of the MR scan take a few days to prepare and then they will be forwarded to your doctor.
| Signed: | Pediatrician |
< prev | top | contents | next >
Table 1.10 Sequence parameters for systems operating at 1.0 Tesla.
These should be adjusted for different field strengths.
| Inversion recovery (IR) sequences: | ||||
| Age | Type | TR | TE | TI |
|---|---|---|---|---|
| 29–34 weeks | IR medium TI | 7000 | 30 | 1500 |
| 35–39 weeks | 6500 | 30 | 1200 | |
| 40 weeks – 3 months | 3800 | 30 | 950 | |
| > 3 months – 24 months | 3500 | 30 | 800 | |
| < 3 months | FLAIR long TI | 6000 | 240 | 2100 |
| > 3 months | FLAIR long TI | 6000 | 160 | 2200 |
| Spin echo sequences at 1.0 Tesla: | TR | TE |
|---|---|---|
| All ages T1 weighted spin echo | 860 | 20 |
| Up to 2 years of age T2 weighted spin echo | 3000 | 120 |
| Fast spin echo (FSE) 16 echo train length | 3500 | 208 |
< prev | top | contents | next >
Table 1.11 Imaging protocols: these will vary from center to center and depend on the clinical problem, the state of the infant, the type and strength of the magnetic field. However, the ones given below have been tried and tested in our department
| T1 weighted spin echo | T2 weighted spin echo | Fast spin echo | Inversion recovery | |
|---|---|---|---|---|
| Slice orientation | Transverse | Transverse | Transverse | Transverse |
| Phase encoding axis | left–right | left–right | left–right | left–right |
| Number of slices | 24 | 24 | 24 | 18 |
| Echo time (TE) | 20 | 120 | 208 | 30 |
| Inversion time (TI) | 1500–800 | |||
| Repeat time (TR) | 860 | 3200 | 3500 | 6000–3500 |
| Field of view | 22–23 | 22–23 | 22–23 | 22–23 |
| Phase resolution | 192 | 128 | 256 | 128 |
| Phase sampling ratio | 256 | 256 | 256 | 256 |
| *Number of signal averages | 2 | 1 or 2 | 4–16 | 1 or 2 |
| Slice thickness | 4mm | 5mm | 4mm | 5mm |
| Receive coil | Smallest available | |||
| *The number of signal averages will depend on time constraints and the size of the receiver coil. | ||||
< prev | top | contents | next >
Table 1.12 Neonatal metal check form to be completed before entry to the scanning room
| Name: | Ward: | |||
| For in-patients (i.e. infants coming from the ward and or the neonatal intensive care unit and supplements metal check form given in Table 1.2) | ||||
| Please check the following items on or in the baby and remove if necessary | ||||
| Action | ||||
|---|---|---|---|---|
| Searle arterial lines (these contain an electronic O2 monitor) | Babies with these in situ must not be put into the scanner | |||
| Scalp needles | Cause susceptibility artifacts which degrade images | |||
| Electronic name tabs | Remove | |||
| Name tabs with metal closures | Remove | |||
| Clothes with metal poppers | Take off | |||
| Ward monitoring leads must be taken off | Take off and replace with MR-compatible leads | |||
| Religious artifacts | Take off | |||
| This is to confirm that the baby named above has been checked and the appropriate action has been taken |
| Signed . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Date . . . . . . . . . . . . . . . . . . . . . |
| Checked by: |
| This form is to be completed before entering the scanning room |
< prev | top | contents | next >
Summary
- ‘Imaging infants is a formidable task to do well’; ‘the least read chapter in most imaging text books is the one on preparation and management’ 3.
- This important group of patients deserve the extra effort and time involved in a technology which continues to evolve and offers diagnostic information not available with any other imaging techniques, and most importantly, without known biological hazard.
- I have included line drawings of John Tenniel in Lewis Carroll’s Alice in Wonderland and Through the Looking-Glass, and What Alice Found There5 in the hope that these ‘images’ will catch your eye and entice you to read this chapter!
< prev | top | contents | next >
Acknowledgments
We are grateful to Macmillan Children’s Books for permission to use the line drawings of John Tenniel from Alice in Wonderland and Through the Looking Glass, and What Alice Found There.
This chapter was written with the advantage of 18 years experience of MRI after 2 years retirement in County Fermanagh, Northern Ireland. It was a task tinged with sadness as well as pleasure and the remembering of the many marvellous and caring people I worked with at Hammersmith Hospital in the Robert Steiner MR unit and the department of Paediatrics. Thank you Frank Doyle, Robert Steiner, Graeme Bydder, David Bryant, David Gilderdale, Lilly Dubowitz, Frances Cowan and Mary Rutherford for all the good times.
< prev | top | contents | next >
References
- American Academy of Pediatrics, Committee on Drugs (1992) Guidelines for monitoring and management of pediatric patient during and after sedation for diagnostic and therapeutic procedures. Pediatrics 89, 1110–1115.
- American Academy of Pediatrics, Committee on Drugs and Committee on Environmental Health (1993) Use of chloral hydrate for sedation in children. Pediatrics 92, 471–473.
- Ball WS Jr (1997) Patient management for neuroimaging. In: Ball WS Jr (Ed.) Pediatric Neuroradiology. Philadelphia, Lippincott–Raven, pp. 3–16.
- Bisset III George S and Ball Jr William S (1991) Preparation, sedation and monitoring of the pediatric patient in the magnetic resonance suite. Seminars in Ultrasound, CT and MRI 12, 376–378.
- Carroll Lewis, with illustrations by John Tenniel (1872) In: Alice in Wonderland, Macmillan, London, pp. 1, 10, 18, 110, 188, and Through the Looking Glass, and What Alice Found There, Macmillan, London, pp. 56.
- Cowan FM, Pennock JM, Hanrahan JD et al. (1994) Early detection of cerebral infarction and hypoxic ischaemic encephalopathy in neonates using diffusion weighted magnetic resonance imaging. Neuropediatrics 25, 172–175.
- Dobbing J and Sands J (1973) Quantitative growth and development of human brain. Arch Dis Child 48, 757–767.
- Greenberg SB, Faerber EN, Aspinall CL et al. (1993) High-dose chloral hydrate sedation for children undergoing MR imaging: safety and efficacy in relation to age. Am J Radiol 161, 639–641.
- Harcke HT, Grissom LE and Meister MA (1995) Sedation in pediatric imaging using intranasal midazolam. Pediatr Radiol 25, 341–343.
- Kanal E, Shellock FG and Talagala L (1990) Safety considerations in MR imaging. Radiology 176, 593–606.
- Louon A and Reddy VG (1994) Nasal midazolam and ketamine for paediatric imaging during computerised tomography. Acta Anaesthesiol Scand 38, 259–261.
- McCarver-May DG, Kang J, Aouthmany M et al. (1996)Comparison of chloral hydrate and midazolam for sedation of neonates for neuroimaging studies. J Pediatr 128, 753–756.
- Noguchi K, Ogawa T, Seto H et al. (1997) Subacute andchronic subarachnoid hemorrhage: diagnosis withfluid-attenuated inversion-recovery MR imaging. Radiology 203(1), 257–262.
- Shellock FG and Kanal E (1996) Appendix 1 list of items tested. In: Magnetic Resonance, Bioeffects, Safety, and Patient management, 2nd edn. Philadelphia, Lippincott–Raven, pp. 179–215. Internet helpline: http://kanal.arad.upmc.edu/mrsafety.html
- Vac-fix available from S&S Xray Products Inc., 1101 Linwood St, Brooklyn NY 11208.
- van der Knaap MS, van Wezel-Meijler G, Barth P et al. (1996) Normal gyration and sulcation in preterm and term neonates: appearance on MR images. Radiology 200, 389–396.
- van der Knaap MS and Valk J (1995) Magnetic Resonance of Myelin, Myelination and Myelin disorders, 2nd edn. Heidelberg, Springer.
- Young IR, Bydder GM and Hajnal JV (1997) Contrast properties of the inversion recovery sequence. In: WG Bradley and GM Bydder (Eds) Advanced MR Imaging Techniques, 1st edn. London, Martin Dunitz, pp. 143–162.